Healthy but hurting: How I got my fibromyalgia diagnosis—doctors, tests and more doctors
Fibromyalgia is no joke: It is important to stay on top of your physical and mental health. Schedule regular check ups to catch anything that may come your way.
Before beginning this week’s topic, I want to say thank you to those who took the time to read my column last week. I received comments from people across the country who also have fibromyalgia. I am grateful for the ability to share my story and for the connections I made with those who also struggle with fibromyalgia. If you would like to go back and read last week’s article, you may find it here.
This week I focus on how I got my fibromyalgia diagnosis. In December 2019, I was at my lowest point. I was exhausted, depressed and in the most physical pain I had ever been in. I was tired of hurting all the time and not having an explanation for it.
Doctors would tell me that I was healthy, but I didn’t feel healthy. In January 2020 I finally decided to commit to figuring out what was wrong with me. Within the next month, I was diagnosed with fibromyalgia, but unfortunately that wasn’t the end of the story.
I went to my primary care physician and explained all of the issues I was dealing with. At that point I had been Googling what my symptoms could possibly be and had come across fibromyalgia. My doctor agreed that it could be fibromyalgia, but could not diagnose me, so she referred me to a rheumatologist which is a doctor that specializes in arthritis and other musculoskeletal conditions and autoimmune diseases.
Despite not being able to diagnose me, my doctor did start me on a prescription to help manage my symptoms called DULoxetine, more commonly known as Cymbalta. I’ll save talking about prescriptions for another week since I have a lot to say about it. That day I also completed a marathon of lab work including CBC and differential, TSH, comprehensive metabolic panel, ANA, C-reactive protein, cyclic citrullinated peptide AB, extractable nuclear antigens, rheumatoid factor and sedimentation rate. By the end of it, I had no blood left.
At my first appointment with my rheumatologist, he asked me to explain my symptoms, tested me for tender points and then talked to me about what fibromyalgia was. It was then that I got my official diagnosis of fibromyalgia.
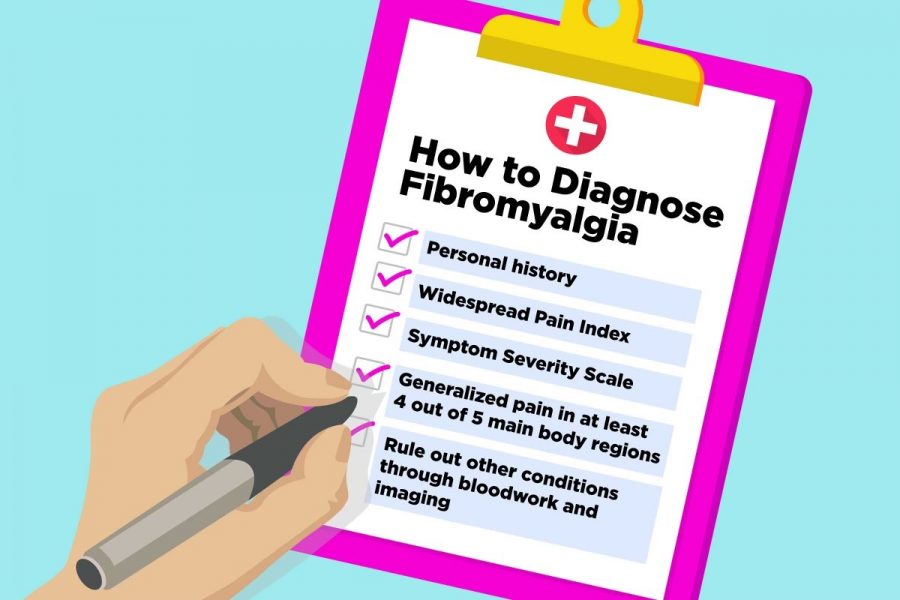
In the past, a tender point exam was performed to help diagnose the condition, but this is no longer required for an official diagnosis.
Fibromyalgia is a unique illness in the sense that it is diagnosed by ruling everything else out. This includes rheumatic diseases such as rheumatoid arthritis,
Sjogren’s syndrome and lupus, as well as neurological disorders such as multiple sclerosis.
Another confounding issue is that fibromyalgia can occur at the same time as other diseases like those listed above. In my case, all of my tests were unremarkable and I was not diagnosed with anything else.
According to Mayo Clinic, “The main factor needed for a fibromyalgia diagnosis is widespread pain throughout your body for at least three months.
To meet the criteria, you must have pain in at least four of these five areas:
Left upper region, including shoulder, arm or jaw
Right upper region, including shoulder, arm or jaw
Left lower region, including hip, buttock or leg
Right lower region, including hip, buttock or leg
Axial region, which includes neck, back, chest or abdomen”
Even though I had my diagnosis after my appointment with my rheumatologist, my tests and appointments didn’t stop there. My rheumatologist referred me to three more doctors: a neurologist, a dermatologist and a gynecologist.
These appointments were required because of symptoms that I had been experiencing that didn’t quite fit the typical fibromyalgia mold. Once again, the idea was to rule out everything else in order to make sure that I only had fibromyalgia.
The list of doctors didn’t stop there either. You see, I had been experiencing some unexplained flushing on my chest and face for some time, which is why I was referred to a dermatologist. The “rash” was red and splotchy, but didn’t itch or burn. In fact, most of the time I didn’t even know it was happening unless I happened to look in the mirror. The dermatologist didn’t have a good explanation for the flushing, so he gave me a couple of creams to try and an order for lab work, but he didn’t tell me what it was for.
Being the control-freak I am, I checked MyChart a few days later and found out it was a 5-HIAA urine lab. This meant nothing to me, but after some Googling, I found out that it measured the amount of serotonin in the body. Seems fine, right? Wrong. The 5-HIAA lab is used to help diagnose and monitor carcinoid tumors. Queue the freakout.
My lab work eventually came back and my 5-HIAA level was 44.4 mg/g when the standard range was 0-6.9 mg/g. Now I was really freaking out.
At that point, it was beyond my dermatologist’s expertise, so I was referred to an oncologist. I’ll save the rest of this story for another week, but just know that it led to more expensive tests, as well as my trip to Mayo Clinic. A little bit over a year later, I finally have confirmation that I do not have a carcinoid tumor, or anything of the sort, and the symptoms I was experiencing were related to fibromyalgia after all.
All of this is to say that pursuing a fibromyalgia diagnosis can result in an extensive and challenging process. It’s not as simple as going to one doctor and getting a diagnosis. If you do seek out a fibromyalgia diagnosis, expect it to be a long process with a lot of doctors and a lot of trial and error, but well worth it in the end.
Your donation will support the student journalists of Washburn University. Your contribution will allow us to purchase equipment and cover our annual website hosting costs.